Drug
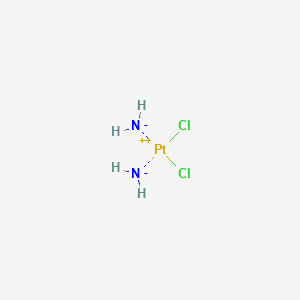
D0029 | Cisplatin
L
L01XA01 Cisplatin
[L01XA] Platinum compounds
[L01X] OTHER ANTINEOPLASTIC AGENTS
[L01] ANTINEOPLASTIC AGENTS
[L] Antineoplastic and immunomodulating agents
| Toxicity | Dose | Time | Species | Model | Method | Action | Positive criterion | Reference |
|---|---|---|---|---|---|---|---|---|
| TRANSMEMBRANE POTENTIAL | 1 or 3 hr | Ishikawa and Caco-2 | JC-10 fluorescent dye | decrease | 299 | |||
| PERMEABILIZATION | U2OS | release of Smac m cherry(IMS-RP probe is a non-functional variant of mitochondrial protein Smac - mCherry fusion protein that acts as an indicator of mitochondrial permeabilization in live cells) | induce | 313 | ||||
| ATP TURNOVER | decrease | 307 | ||||||
| GLUCOSE GALACTOSE IC50 RATIO | 1 | LUHMES (Lund human mesencephalic) cells | Glc–Gal–NeuriTox assay | Negative | EC25(NA) [Glc/Gal] | 326 | ||
| SHAPE | 197 | |||||||
| MITOCHONDRIAL DYNAMICS | 3 mg/kg bodyweight | twice a week for 2 weeks | Mouse | Mouse tibial nerves and dorsal root ganglia (L1–L4) | 247 | |||
| ROS PRODUCTION | 84.96 ± 3, 158.9 ± 8.2, 372.7 ± 17.5 and 499.5 ± 15.1 μM | 24 hr | Ishikawa, MDA-MB-231, PC-3 and Caco-2 | Intracellular ROS (a) and mitochondrial superoxide were measured by fluorescence intensity of H2DCFDA and MitoSOX respectively. | increase | IC50 | 299 | |
| ROS PRODUCTION | 150 µM | 24hr | U2OS | U2OS cells stably expressing mt-roGFP and HyPer-red targeted at mitochondria | increase | 313 | ||
| ROS PRODUCTION | Increase | 307 | ||||||
| MITOCHONDRIAL DNA METABOLIC PROCESS | 24 hr | Caco-2 and Ishikawa cells | Relative quantification of mtDNA copy number was measured using the QuantiTect SYBR Green PCR kit | decrease | 299 | |||
| MITOCHONDRIAL DNA DAMAGE | Increase | 307 | ||||||
| APOPTOSIS | 24 hr | Ishikawa and Caco-2 | WB was performed to measure the BCL-XL and released cytochrome c proteins from mitochondria; Caspase-3/7 activity was measured using the Caspase-Glo 3/7 reagent from the ApoTox-Glo Triplex Assay kit | induce | 299 | |||
| Target | Dose | Time | Species | Model | Method | Action | Positive criterion | Reference |
|---|---|---|---|---|---|---|---|---|
| Reactive oxygen species | increase | 307 | ||||||
| Organism | Test type | Route | Dose (normalized dose) | Effect | Source |
|---|---|---|---|---|---|
| guinea pig | LD50 | intraperitoneal | 9700ug/kg (9.7mg/kg) | sense organs and special senses: change in acuity: ear | Toxicology and Applied Pharmacology. Vol. 33, Pg. 320, 1975. |
| dog | LDLo | intravenous | 2500ug/kg (2.5mg/kg) | Toxicology and Applied Pharmacology. Vol. 25, Pg. 230, 1973. | |
| mouse | LD50 | intramuscular | 17900ug/kg (17.9mg/kg) | Yakuri to Chiryo. Pharmacology and Therapeutics. Vol. 10, Pg. 723, 1982. | |
| human | TDLo | intravenous | 1500ug/kg/6D- (1.5mg/kg) | Cancer Chemotherapy Reports, Part 1. Vol. 57, Pg. 191, 1973. | |
| human | TDLo | intravenous | 500ug/kg/13D- (0.5mg/kg) | Cancer Treatment Reports. Vol. 62, Pg. 693, 1978. | |
| rat | LD | unreported | > 5mg/kg (5mg/kg) | kidney, ureter, and bladder: "changes in tubules (including acute renal failure, acute tubular necrosis)" | Journal of Toxicological Sciences. Vol. 24, Pg. 337, 1999. |
| human | TDLo | intravenous | 72mg/kg/25D-I (72mg/kg) | gastrointestinal: nausea or vomiting | Cancer Treatment Reports. Vol. 62, Pg. 1591, 1978. |
| mammal (species unspecified) | LDLo | intravenous | 8mg/kg (8mg/kg) | gastrointestinal: nausea or vomiting | Yakuri to Chiryo. Pharmacology and Therapeutics. Vol. 28(4), Pg. 285, 2000. |
| mouse | LD50 | intravenous | 11mg/kg (11mg/kg) | Archives of Toxicology, Supplement. Vol. 7, Pg. 90, 1984. | |
| mouse | LD50 | parenteral | 22mg/kg (22mg/kg) | International Journal of Radiation Oncology, Biology, Physics. Vol. 5, Pg. 1417, 1979. | |
| rat | LD50 | oral | 25800ug/kg (25.8mg/kg) | Yakuri to Chiryo. Pharmacology and Therapeutics. Vol. 10, Pg. 723, 1982. | |
| man | TDLo | parenteral | 2140ug/kg/5D- (2.14mg/kg) | kidney, ureter, and bladder: "changes in tubules (including acute renal failure, acute tubular necrosis)" | Nippon Naika Gakkai Zasshi. Journal of the Japanese Society of Internal Medicine. Vol. 72, Pg. 1426, 1983. |
| mouse | LD50 | intraperitoneal | 6600ug/kg (6.6mg/kg) | Journal of Medicinal Chemistry. Vol. 34, Pg. 414, 1991. | |
| rat | LD50 | intramuscular | 9200ug/kg (9.2mg/kg) | Yakuri to Chiryo. Pharmacology and Therapeutics. Vol. 10, Pg. 723, 1982. | |
| human | TDLo | intravenous | 2500ug/kg (2.5mg/kg) | Cancer Chemotherapy Reports, Part 1. Vol. 59, Pg. 647, 1975. | |
| mouse | LD50 | subcutaneous | 13mg/kg (13mg/kg) | Journal de Pharmacie de Belgique. Vol. 41, Pg. 286, 1986. | |
| mouse | LD50 | unreported | 10900ug/kg (10.9mg/kg) | Gan to Kagaku Ryoho. Cancer and Chemotherapy. Vol. 13, Pg. 280, 1986. | |
| rat | LD50 | intraperitoneal | 6400ug/kg (6.4mg/kg) | Journal of Toxicological Sciences. Vol. 18, Pg. 31, 1993. | |
| child | TDLo | unreported | 19200ug/kg/12 (19.2mg/kg) | sense organs and special senses: change in acuity: ear | Journal of Pediatrics. Vol. 103, Pg. 1006, 1983. |
| frog | LD50 | parenteral | 17mg/kg (17mg/kg) | Journal of Comparative Pathology. Vol. 103, Pg. 387, 1990. | |
| mouse | LD50 | oral | 32700ug/kg (32.7mg/kg) | Kiso to Rinsho. Clinical Report. Vol. 15, Pg. 5669, 1981. | |
| monkey | LDLo | intravenous | 250ug/kg (0.25mg/kg) | Cancer Vol. 33, Pg. 1219, 1974. | |
| human | TDLo | intradermal | 40ng/kg (0.00004mg/kg) | Cancer Research. Vol. 35, Pg. 2766, 1975. | |
| man | TDLo | intravenous | 2140ug/kg/5D- (2.14mg/kg) | kidney, ureter, and bladder: "changes in tubules (including acute renal failure, acute tubular necrosis)" | Japanese Journal of Medicine. Vol. 23, Pg. 283, 1984. |
| rat | LD50 | subcutaneous | 8100ug/kg (8.1mg/kg) | Kiso to Rinsho. Clinical Report. Vol. 15, Pg. 5669, 1981. | |
| mouse | LD50 | intraperitoneal | 27mg/kg (27mg/kg) | Chemico-Biological Interactions. Vol. 5, Pg. 415, 1972. | |
| rat | LD50 | intravenous | 8mg/kg (8mg/kg) | kidney, ureter, and bladder: other changes | JNCI, Journal of the National Cancer Institute. Vol. 67, Pg. 201, 1981. |
| AB00642613-02 | AB00642613_03 | AC-2109 |
| AKOS025401526 | BCP9000536 | BDBM50028111 |
| BRD-K69172251-001-01-4 | CAS-15663-27-1 | CS-1122 |
| Cisplatin(cis-Diammenedichloroplatinum) | DB00515 | DSSTox_CID_4983 |
| DSSTox_GSID_24983 | DSSTox_RID_77611 | DTXSID4024983 |
| FT-0082333 | FT-0623946 | HMS3268F06 |
| HMS3654E14 | HY-17394 | NCGC00090759-01 |
| NCGC00090759-02 | NCGC00090759-03 | NCGC00260049-01 |
| NCGC00263537-01 | NSC-131558 | NSC-241517 |
| NSC131558 | NSC241517 | Neuro_000055 |
| Platinum (II) complex | Platinum(IV) Complex | Platinum, diamminedichloro- |
| Pt(II) Complex | Replaced CAS registry number(s): 14283-03-5 | SW222225-1 |
| Tox21_111011 | Tox21_111011_1 | Tox21_113470 |
| Tox21_202500 | camphorato platinum complex derivative | cis-Diaminedichloroplatinum |
| cis-Diammine-dichloroplatinum(II) | cis-Diamminedichlorplatine | cis-Dichlorodiamine platinum |
| cis-Platinum diamminedichloride | cis-Platinum(II) | cis-diamminedichloroplatinum(II)(cis-DDP) |
| cisplatin complex | dichloromethanediamine(platinum complex) | dichloroplatinumdiamine |
| trans-Diaminedichloroplatinum | trans-dichlorodiammineplatinum.(transplatin) |
1. Vuda et al. (2016)
2. LeDoux et al. 1992
3. Meyer et al. (2017)
4. Bobylev et al. (2017)
5. Meyer et al. (2013)